The spin-outs changing our world

From pioneering synthetic bone graft materials to a miniaturised cold atom system, breakthroughs across the science and engineering spectrum are creating spin-outs that are transforming lives.
These spin-outs have the potential not only for huge commercial success, but also to redefine how research, patient care and product development is handled in the future. Here are some success stories of spin-outs from Science and Engineering South member institutions.
King’s College London: using AI to reduce risks for patients in surgery

Innovations in healthcare shouldn’t come at a cost to patient safety, and King’s spin-out Cydar Medical is tackling this using disruptive AI technology.
For patients needing endovascular aortic surgery, time and precision are of the essence. Minimally invasive surgery is quicker and safer but previously to do so required more X-ray images ahead of surgery, increasing the risk of exposing the patient to high doses of harmful ionising radiation and kidney-toxic contrast agents
Devised by researchers at King’s College London, Cydar uses an AI-driven image guidance system called Cydar-EV that combines different types of imagery to reduce the need for radiation exposure and shorten the duration of surgery. The School of Biomedical Engineering and Imaging Science created Cydar-EV by successfully aligning 3D CT images – also known as computed tomography – and 2D X-ray images, a crucial component in the success of the surgery.
In the past, the planning of such surgeries used high-resolution 3D images from preoperative CT scans, but the surgery itself was performed using 2D X-ray fluoroscopy. This loss of dimensional spatial information makes it more complex for the surgeon as they must try to visualise the 3D anatomy to accurately position the device.
Cydar-EV matches CT and X-ray images based on their similarity and automatically links them using a process called image registration. The technology is proven to be fast, accurate and robust and helps to improve
patient survival rates, reduce postoperative complications, and shorten the lengths of hospital stay.
By 2020, more than 2,000 patients had been treated using Cydar-EV and with it, Cydar became the first company in the world with a European CE-marked and US FDA-cleared product using cloud and AI technology to inform and influence surgery in real-time.
University of Southampton: the future of quantum technology and pioneering software for prosthetics

Southampton has been linked to two spin-outs making serious waves in the field of healthcare and quantum mechanics.
Dr Joshua Steer has created Ampscan, biomechanical simulation software that is revolutionising the fit and comfort of artificial limbs. Built using the Python programming language, this open-source software was created while Dr Steer was working on his PhD in the Bioengineering Sciences Research Group.
In 2020, the team spun out the technology and created Radii Devices, and two years on it has five employees including two PhD graduates and one undergraduate.
Today, the software is used by research groups in the UK, USA, Italy, Singapore, Canada and Australia.
In collaboration with the university and multiple NHS prosthetic clinics, the spin-out is about to embark on clinical trials of its software to improve prosthetic limb fitting.
In Southampton’s School of Physics and Astronomy, the spin-out Aquark Technologies, is headed up by Dr Andrei Dragomir, Dr Alexander Jantzen and their small team.
Sitting right on the brink of a revolution in quantum technology, Aquark is developing a miniaturised cold atom system, no bigger than a matchbox.
The aim? To vastly reduce the size of this core component of quantum technology. If achieved, the possibilities are endless. From minimising the system size of an entire lab to the palm of your hand to creating a global navigation system with pin-point accuracy without a satellite connection.
University of Cambridge: reducing environmental pollution in the water supply industry
Seven UK water companies that collectively supply 34.7 million people with drinking water have signed up to trial BioBullets, the product of University of Cambridge spin-out BioBullets Ltd. Created by Dr David Aldridge and Professor Geoff Moggridge, BioBullets were developed as an efficient and safe way to reduce the environmental pollution caused by non-native mussels and clams.
Unlike native freshwater mussels that tend to live in riverbeds, many invasive mussels – such as the zebra mussel – attach themselves to hard surfaces leading to biofouling: the accumulation of mussels in water pipes. This causes major problems for water companies including the blocking of raw water supply mains and raw water monitoring lines, which affects the quality of supply to customers. These unassuming shellfish cost the UK water supply industry £8m each year and are driving dramatic ecosystem shifts with a decline in native biodiversity. On top of their natural pollution, previous treatments have involved the continuous pumping of chlorine into waterways, which is toxic to humans and other animals, expensive and hazardous to store.
Dr Aldridge and Professor Moggridge created the simple, but effective BioBullet by taking advantage of the zebra mussels’ fussy eating habits. When the animal tastes something it doesn’t like – like chlorine for example – it can bind the substance in mucus and expel it.
To get around this natural defence system, the BioBullet particles are coated in a fatty substance which the mussel will detect as being food and ingest. Each BioBullet contains a salt blend which is lethal to the invasive mussel species, but completely harmless to native mussels. The formulation then naturally dissolves without affecting water quality.
Water companies are understandably excited by this technology, and have identified that using a BioBullet solution is 69% cheaper than the alternative, more hazardous control methods. This popularity has led to job creation and commercial benefits at the new BioBullet manufacturing plant in Bristol.
Queen Mary University of London: improving the quality of life for patients post-bone graft surgery
Research into the next generation of synthetic bone graft material has seen a range of scientists, researchers, academics and industry professionals come together to share their skills and resources. The resulting material was one of seven innovations presented on Royal Mail Stamps celebrating 50 years of British engineering.
Since 2000, Dr Karin Hing has been building on years of bone graft research under the directorship of Professor William Bonfield, Professor Serena Best and Professor Iain Gibson. This research explored graft chemistry, and the ability of a synthetic bone graft to stimulate bone regeneration.
Along with her team of academics, Dr Hing discovered that in order to stimulate natural bone regeneration, the structural composition of the synthetic graft pores needed to be the right size for new bone to grow in to , allowing the exchange of cells and nutrients via blood vessels to nourish and sustain healthy bone tissue.
To commercialise this research, the ApaTech™ spin-out was established in 2001, and purchased by Baxter International in 2010 to broaden its scope. The result of this was the synthetic bone graft substitute Inductigraft™ (or AltaPore™ in the US), which clinical trials have shown to be as effective as an autograft with one significant advantage – the patient wouldn’t need additional surgery to harvest the autograft itself.
Inductigraft™ and AltaPore™ have transformed the lives of some 400,000 patients in 30 countries to date, with the grafts used in around 24,000 operations a year. The research has led to safer and more reliable surgery, improved outcomes and better quality-of-life for patients after surgery – with 98.9% fusion rates. The materials are currently worth an estimated US$3.78bn.
University College London: monitoring brain activity with wearable imaging devices

Wearable devices are becoming increasingly commonplace but UCL spin-out Gowerlabs has taken this one step further. They have created LUMO, the world’s first commercially available wearable high-density brain imaging device.
Dr Nick Everdell and his multidisciplinary team, which includes Professor Jeremy Hebden and Dr Robert Cooper of UCL’s Biomedical Optics Research Laboratory as well as Dr Samuel Powell from the University of Nottingham, have made significant improvements to the technology known as Diffuse Optical Tomography (DOT). This technology, also known as functional near-infrared spectroscopy (fNIRS), produces images of brain activity by shining low levels of near-infrared light through the scalp and skull. The light is non-ionizing, and so is completely safe.
Using this technique, the team’s aim was to develop a high-density, wearable and wireless device that would significantly increase imaging resolution for applications in real-world settings. The result was LUMO – the first ever modular high-density DOT system. It is able to generate much higher quality images than its predecessors. Its modularity allows for flexible configuration to suit the brain imaging task at hand. It has done away with the need for heavy and bulky optical fibres as the light sources and detectors are placed directly on the scalp.
The result is a system with greatly improved signal quality and a huge range of applications. Essentially, it has allowed brain activity to be imaged with high resolution outside of the laboratory for the first time.
Understandably, this major upgrade to the technology immediately attracted tech giants, and it is now being used by Facebook, Apple, and many other research institutions and universities.
Imperial College London: making a safer, more efficient oil and gas industry
Two state-of-the-art systems developed by academics at Imperial College London have saved the oil and gas industry in excess of US$8bn every year by transforming how corrosion is managed.
The systems monitor pipework wall thickness in real-time – one for high temperatures up to 6,000C and another for temperatures up to 3,000C. The data from these readings is transmitted directly to the plant control room, allowing staff to react quickly and effectively to changes to the environment. It also helps to improve on-site safety by allowing staff to optimise their feedstock while reducing the use of corrosion inhibitor chemicals, which carry higher risks to human safety. These battery-operated systems provide maintenance-free operation for up to ten years.
The result of this research by Professor Peter Cawley and Frederic Cegla in the Department of Mechanical Engineering, is the spin-out Permasense Ltd, which was sold to Emerson in 2016. The spin-out now employs 52 staff in the UK with BP and other major clients using the technology as a key tool in their strategies for corrosion prevention. Currently, there are more than 20,000 corrosion sensors in some 200 sites world-wide, generating more than US$72m worth of revenue for the company over the current REF period.
University of Oxford: revolutionising patient care in mental health settings
Oxehealth is a spin-off venture from the Institute of Biomedical Engineering at Oxford University and is changing the face of patient care across the world.
Much of the research of Institute founder Professor Lionel Tarassenko, has focused on patient monitoring and his work has had a major, positive impact on the management of long-term health conditions.
Professor Tarassenko’s research group was initially examining methods and algorithms for the non-contact monitoring of vital signs in mental healthcare settings. These environments often require close supervision of patients but with a need for considered privacy throughout treatment and care. The group discovered that video cameras could easily be converted into health monitors, allowing real-time estimation of heart and breathing rates with clinical-level accuracy. The Oxevision spin-out was one product of the research, and has grown to be internationally successful from its initial application in technology such as baby monitors.
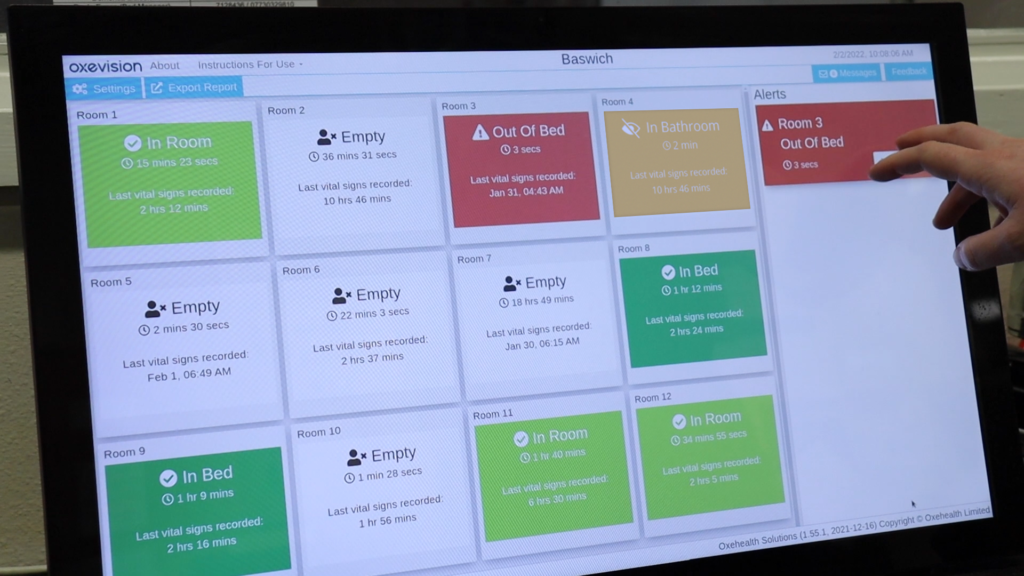
The software uses computer vision algorithms which enable patient location and motion to be quantified. An optical sensor, which uses a video camera plus infrared illumination mounted on a wall, monitors a patient in a bedroom or seclusion room 24/7. No equipment is in contact with the patient and staff interact with the system via a monitor in the nurses’ station or portable tablet devices. This allows care staff to provide better quality of care for patients and helps to identify incidents such as a fall for an elderly patient without constant intrusion.
Oxevision is the world’s first CE-marked continuous medical-grade, vital-sign monitoring system that uses low-cost digital video cameras. To date, the software (called Oxevision) has been installed in 30% of mental health NHS Trusts in England and two separate sites in Scandinavia, with £2.08m in annual recurring revenue for Oxehealth. The resulting installation has resulted in better patient safety – including a 82% decrease in harmful falls for elderly patients, plus less intrusive observations and improved patient privacy.

